By: Susan Richardson, PhD, Research Analyst, National Improvement Partnership Network
Even before the pandemic, there was a rising concern for adolescent and young adult mental health in the United States.[1] Data from the 2019 Youth Risk Behavior Survey (YRBS) showed that 36.7% of high school students reported being sad or hopeless almost every day for two weeks in a row, preventing them from doing some of their usual activities.[2]
Then, in the early winter of 2020, being able to do “usual activities” took on a new meaning as the COVID-19 pandemic dramatically changed daily life. As schools closed and stay at home orders become the norm, adolescents became isolated from peers and their communities. Mental health-related emergency department visits increased[3] among adolescents, along with a growing awareness of the need to monitor the mental health of children and adolescents during the pandemic.
To measure the impact of the pandemic on adolescent health, the CDC developed the Adolescent Behaviors and Experiences Survey (ABES). This one-time survey was modeled after and included many of the questions from the YRBS, like the one above about feeling sad or hopeless, but also included specific questions about students’ perceptions of how the pandemic impacted their life. One of these pandemic-specific questions asked students about their mental health during the pandemic. The survey was administered January-June 2021 to a nationally representative sample of students in grades 9-12 at public and private schools.
The CDC recently released findings* from the ABES and found that:
- 37.1% of high school students reported that during the COVID-19 pandemic, their mental health was poor (poor mental health described as including stress, anxiety, and depression) most of the time or always.
- 44.2% agreed that they had ever in the past year (i.e., thinking about 2020) felt so sad or hopeless almost every day for two weeks in a row that it impacted their usual activities.
Two of the ABES questions about mental health:
- During the past 12 months, did you ever feel so sad or hopeless almost every day for two weeks or more in a row that you stopped doing some usual activities? (Yes or No)
- During the COVID-19 pandemic, how often was your mental health not good? (Poor mental health includes stress, anxiety, and depression.) (Never, Rarely, Sometimes, Most of the time, Always)
Findings from the survey also highlighted protective factors for students during these challenging times:
- Most students (71.8%) reported that they felt virtually connected to family, friends, and other groups, but only about half (46.6%) of students agreed or strongly agreed that they felt connected to persons at school.
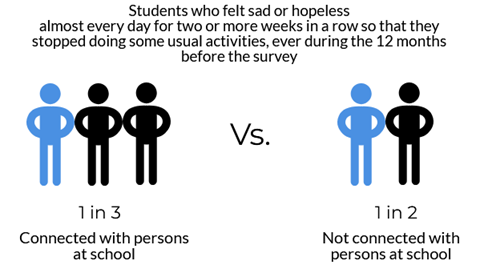
- Among students who felt connected to persons at school, only about one-third (35.4%) agreed or strongly agreed that they had persistent feelings of sadness or hopelessness. By comparison, half (52.9%) of students without that connection agreed or strongly agreed with this statement.
- Fewer students who felt connected to persons at school reported poor metal health during the pandemic (28.4%) compared to students that did not feel connected (45.2%).
- Students who felt virtually connected to friends, family, or other groups via electronics (not counting school time) also had a lower prevalence of persistent sadness or hopelessness when compared to students who are not virtually connected to friends, family, or other groups via electronics (41.9% vs. 51.7%). Additionally, student who felt virtually connected to friends, family, or other groups via electronics reported a lower prevalence of poor mental health during the pandemic than student who did not feel virtually connected to friends, family, or other groups via electronics (35.5% vs. 42%), though the differences between the groups was smaller than what was observed among students feeling a connection with persons at school or not.
Given the lower incidence of self-reported poor mental health among those with school connectedness, future efforts to foster connections within schools is an important goal to strive for. Also, it should be noted that students’ self-reported connection to persons at school varied by their sex, race and ethnicity, and/or sexual identity. Programs designed to increase adolescents’ connectedness to schools should consider how different student groups would experience and respond to different interventions. The CDC, the American Psychological Association (APA), and the National Center for School Mental Health (NCSMH) each provide ideas and resources that can be implemented in communities to increase adolescents’ feelings of connection. In addition, the Adolescent & Young Adult Health National Resource Center has hosted learning sessions for participants of the Adolescent & Young Adult Behavioral Health Collaborative Improvement and Innovation Network that share evidence-based strategies for developing comprehensive school mental health services. View the recorded learning sessions by clicking the links below:
- Schools as a Setting for Mental Health Care for Adolescents & Young Adults
- Comprehensive School Mental Health: Planning for the School Year During COVID-19
*The full report of findings from the ABES survey can be reviewed here: Jones SE, Ethier KA, Hertz M, et al. Mental Health, Suicidality, and Connectedness Among High School Students During the COVID-19 Pandemic — Adolescent Behaviors and Experiences Survey, United States, January–June 2021. MMWR Suppl 2022;71(Suppl-3):16–21. DOI: http://dx.doi.org/10.15585/mmwr.su7103a3external icon.
References
[1] Cori M. Green, Jane Meschan Foy, Marian F. Earls, COMMITTEE ON PSYCHOSOCIAL ASPECTS OF CHILD AND FAMILY HEALTH, MENTAL HEALTH LEADERSHIP WORK GROUP, Arthur Lavin, George LaMonte Askew, Rebecca Baum, Evelyn Berger-Jenkins, Thresia B. Gambon, Arwa Abdulhaq Nasir, Lawrence Sagin Wissow, Alain Joffe; Achieving the Pediatric Mental Health Competencies. Pediatrics November 2019; 144 (5): e20192758. 10.1542/peds.2019-2758
[2] Centers for Disease Control and Prevention (CDC). 1991-2019 High School Youth Risk Behavior Survey Data. Available at http://yrbs-explorer.services.cdc.gov/. Accessed on 5/9/2022
[3] Leeb RT, Bitsko RH, Radhakrishnan L, Martinez P, Njai R, Holland KM. Mental Health–Related Emergency Department Visits Among Children Aged <18 Years During the COVID-19 Pandemic — United States, January 1–October 17, 2020. MMWR Morb Mortal Wkly Rep 2020;69:1675–1680. DOI: http://dx.doi.org/10.15585/mmwr.mm6945a3external icon
