Integrating Maternal and Child Health (MCH) Considerations in Emergency Preparedness and Response (EPR) Efforts
Strategies for Enhancing Public Health Approaches
Course objectives
After completing the course, learners will be able to:
- Describe the implications for maternal and infant health during public health emergencies.
- Identify opportunities to gather epidemiologic and surveillance data on women of reproductive age and infants to guide public health emergency preparedness and response actions.
- Identify best practices for communicating with diverse audiences about the needs of women of reproductive age and infants across all phases of emergency management.
- Describe activities that promote coordination with existing programs, interventions, and policies that can protect maternal and infant health during emergencies.
Intended audiences
This course is meant for people who: (a) work in or intersect with public health at any level of government, (b) are poised to influence outcomes for women of reproductive age, specifically pregnant and postpartum people, and infants, and (c) provide direct, enabling, or system-level support to communities during emergencies.
Prerequisite knowledge and skills
- Interest in how to elevate and more equitably address maternal and infant health needs during all types of emergencies.
- Ability to navigate a web-based learning course with multimedia (video clips, .pdf documents, hyperlinks to external websites) and interactive (i.e., “try it”) components.
Recommended knowledge and skills
Completion of the Strategies for Initiating and Sustaining Critical Partnerships .
Instructions
The modules in this course are intentionally sequenced to support learning; each module builds on content presented in the previous module. At points, you will be prompted to stop and complete reflection and/or application activities (e.g., action planning) in a participant workbook. This is an accessible, fillable .pdf document that you can save to your desktop, add to as you complete the course, and keep for later reference. While not required, the workbook promotes active engagement with course content and application of learning to your professional role(s).
Anticipated time to complete: 90 minutes
Module 1: Introduction
What are public health emergencies?
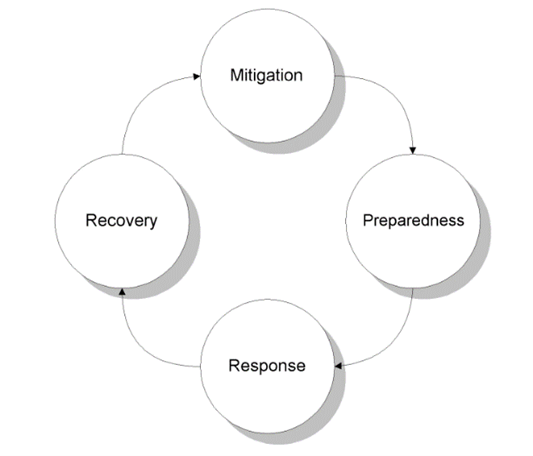
Mitigation: Actions taken to prevent and reduce the overall cause and impact of disasters including, but not limited to: constructing levees or other permanent barriers to control flooding, tying down buildings with ground anchors to withstand high winds, and buying insurance policies.
Preparedness: Planning, training, and education for disaster events that cannot be mitigated or prevented, such as participating in disaster drills and tabletop exercises, and developing preparedness plans for what to do in case of a disaster.
Response: Actions taken in the duration or immediate aftermath of a disaster, including implementing disaster response plans, addressing public health concerns such as disease spread and food contamination, and conducting search and rescue missions.
Recovery: Efforts occurring when regular operations and activities are re-established. The recovery period can often be prolonged and includes activities such as preventing or alleviating financial burden, rebuilding damage structures, and starting mitigation activities to lessen vulnerability during future disasters.
Why focus on women of reproductive age, specifically pregnant and postpartum people, and infants?
In this video clip (3:38), Dr. Wanda Barfield, Director of the Division of Reproductive Health at the CDC, addresses the importance of centering women of reproductive age – specifically pregnant and postpartum people, and infants – in emergency preparedness and response. She provides poignant examples of successes and unique challenges for these populations that surfaced during multiple types of recent emergencies.
Other reasons why we choose to center these populations include:
- Federal legislation identifies pregnant and postpartum women and infants as populations with special clinical considerations in public health emergencies;
- People who are pregnant or postpartum may experience higher rates of poor reproductive outcomes during and after disasters, such as miscarriages, premature deliveries, cases of intrauterine growth restriction (IUGR), low birth weight infants, sexual violence, and lack of access to contraception2;
- Pregnant, postpartum, and breastfeeding people and infants may be uniquely impacted by public health issues resulting from disasters, such as contaminated food and water sources2; and
- Focusing on the specific circumstances experienced by people who are pregnant and postpartum and infants contributes to an “all hazards approach” by ensuring that health and other systems have the capacity to address the broadest possible range of emergency needs. This includes preventing excess adverse outcomes and exacerbations of existing health disparities in pregnancy-related morbidity and mortality.
How can preparedness and response activities be platforms for evidence-based, equity-centered practice?
Disasters occur within a specific context based on a community’s geographic, cultural, demographic, political, and historical characteristics, which produce unique considerations for each1.. They require tailored solutions. As an example, the Stafford Act requires FEMA assistance be delivered in an equitable manner without discrimination on the grounds of race, color, religion, nationality, sex, age, disability, language accessibility, or economic status. However, this cannot be done through a one-size-fits-all approach.
Executive Order 13985 (January 20, 2021) defines equity as “the consistent and systematic fair, just, and impartial treatment of all individuals, including individuals who belong to underserved communities that have been denied such treatment, such as Black, Latino, and Indigenous and Native American persons, Asian Americans and Pacific Islanders and other persons of color; members of religious minorities; lesbian, gay, bisexual, transgender, and queer (LGBTQ+) persons; persons with disabilities; persons who live in rural areas; and persons otherwise adversely affected by persistent poverty or inequality.”
Watch this video clip (2:30) that describes the critical need to apply equity frameworks across all phases of emergency management. This perspective is reinforced by federal entities, such as the Federal Emergency Management Agency (FEMA). Pages 9-13 of their strategic plan identifies opportunities to “instill equity as a foundation of emergency management,” such as:
- Understand the factors that affect a community’s resilience and vulnerability to disasters;
- Proactively and continuously engage state, local, tribal, and territorial partners, local community leaders, and other community representatives to gain insight into how programs can better serve them;
- Make space to invite and elevate diverse voices, and to foster mutual understanding and respect for [different] perspectives and experiences;
- Deliberately [define] what success looks like for each user of each program in a manner that can be consistently measures;
- Routinely evaluate programs and policies for disparities in outcomes; and
- Conduct ongoing equity-based evaluations across programs, as well as partner with external organizations experienced in this work.
How is individual leadership development across roles and settings necessary for capacity building?
WATCH:This video clip (4:47) connects gains in individual knowledge, skills, and abilities to collective emergency response capability. It references two federal guidance documents from the fields introduced above that learners are encouraged to explore in greater depth. Presenter: Mikayla Frye, Program Manager for Workforce Development and Capacity Building, AMCHP.
- Public Health Emergency Preparedness and Response Capabilities: National Standards for State, Local, Tribal, and Territorial Public Health, 2018 Update (Centers for Disease Control and Prevention)
- Maternal and Child Health Leadership Competencies, Version 4.5 (Health Resources and Services Administration)
Module 2: The Public Health Emergency Preparedness and Response Checklist for Maternal and Infant Health
Originally designed to guide interdisciplinary teams from U.S. states, territories, or freely associated states participating in AMCHP’s Emergency Preparedness and Response Action Learning Collaborative, this Checklist is intended to augment the capacity of all jurisdictions to ensure that women of reproductive age, especially pregnant and postpartum people, and infants are planned for in the event of emergencies – including multiple emergencies with intersecting impacts. This tool was repeatedly recognized by participants as a useful tool for prioritizing strategies and selecting action items.
In this video clip (8:53), Dr. Marianne Zotti provides an overview of the Checklist that includes background, alignment with federal emergency preparedness guidance, a brief description of the four overarching strategic areas, and how to read and use each Checklist component.
Later in the course, you will complete reflection and application activities that require you to interact with both the Checklist and Action Item Cards (the structure of these are described beginning at 7:51 of the previously referenced video clip) that elaborate on planning and implementation considerations associated with each activity. You will be able to “jump” to and from these as you complete the activities using the workbook, but it is recommended that you download these for easy access.
Module 3: Develop Strategies to Gather Epidemiologic/Surveillance Data on Women of Reproductive Age and Infants to Guide Action (Checklist Strategy #2)
Before starting this module, make sure you’ve downloaded and/or printed both the Checklist and Action Implementation Card for easy reference.
Overview
This video clip (2:46) introduces the presenters of subsequent related content and offers a “big picture” perspective on the significance of this strategy in building overall preparedness and response capacity. Presenter: Mikayla Frye, Program Manager for Workforce Development and Capacity Building, AMCHP.
Activities within Strategy #2 support two (2) PHEP capabilities:
- Community Preparedness
- Public Health Surveillance and Epidemiological Investigation
Didactic Breakdown of Select Activities
Watch the following video clips to learn about a few activities included in the checklist for Strategy #2. You can find the complete list of Checklist activities that support Strategy #2 in the Checklist document offered for download at the start of this course.
Centering Equity in Practice
Addressing maternal and infant health needs in planning for and responding to emergencies cannot be disconnected from the broader pursuit of equitable outcomes for all. This video clip (1:42) demonstrates how to apply an equity lens in implementing a specific capacity building activity (S2-A5). A primary takeaway is to recognize and address the structural limitations and unintentional biases in surveillance systems and practices. Presenter: Ben Kaufman, Associate Director for Workforce Development and Capacity Building, AMCHP.
Implementation Support Spotlight: Surveillance Tools
Please select either (a) PRAMS or (b) the CDC Pregnancy Estimator tool to explore in more detail or choose to explore both if you are interested and time permits.
PRAMS
EXPLORE: On the PRAMS page of the CDC website, you can view the core and supplemental questionnaires, learn about methodology, see which jurisdictions participate, access released data, read success stories, and more.
WATCH: In this video clip (3:39), Penelope Strid, MPH, CDC epidemiologist, describes what PRAMS is and the eight-part preparedness question that is currently offered as standard. She briefly reviews how this was implemented and analyzed in two states, Hawaii and Tennessee, including how Hawaii stratified their analyses.
CDC Pregnancy Estimator Tool
EXPLORE: On the DRH EPR Tools and Resources page of the CDC website, you can scroll down to the “Pregnancy Estimator” section to find .pdf copies of a simulated example and point-in-time calculator form, as well as a geographic calculator (.xlsx) to generate estimates for your jurisdiction. There is also a brochure (link) that explains the tool in more detail.
WATCH: In this “Voices from the Field” video clip (0:43), Andrea Lenartz, MPH, former CSTE Applied Epidemiology Fellow for Maine shows how they use the Pregnancy Estimator Tool and other sources (e.g., Social Vulnerability Index) to visualize data they are asked to gather in S2-A1.
Supplemental Resources
| Title | Author(s) | Format | Purpose |
| Emergency Preparedness in Tennessee Women with a Recent Live Birth | Miller, A. M., Galang, R. R., Hall, L. E., Strid, P., Leverett, U., & Ellington, S. R. | Scholarly article (link) from a 2023 issue of Maternal and Child Health Journal. | The implementation and analysis of PRAMS in Tennessee may be of interest to those supporting highly rural populations. |
| Disaster Preparedness Among Women with a Recent Live Birth in Hawaii – Results from the Pregnancy Risk Assessment Monitoring System (PRAMS), 2016. | Strid, P., Fok, C. C. T., Zotti, M., Shulman, H. B., Awakuni, J., House, L. D., Morrow, B., Kern, J., Shim, M., & Ellington, S. R. | Scholarly article (link) from a 2022 issue of Disaster Medicine and Public Health Preparedness. | The implementation and analysis of PRAMS in Hawaii may be of interest to those interested in data stratification practices. |
| Social Vulnerability Index (SVI) | CDC’s Agency for Toxic Substances and Disease Registry (ATSDR) | Interactive page (link) on a federal website. | Shows how 16 U.S. Census variables can help government officials identify communities that may need support before, during, or after emergencies. |
| Reproductive Health and Disasters (RHAD) Assessment Toolkit 2.0 | Council of State and Territorial Epidemiologists (CSTE) | Interactive page (link) from a national association website. | Assist agencies or communities with assessing the reproductive health needs of women aged 15-44, pregnant and postpartum women, and infants less than 1 year old affected by disasters. |
| Health Indicators for Disaster-Affected Pregnant Women, Postpartum Women, and Infants | CDC | 56-page .pdf document (link). | Identify salient conditions to be monitored via surveillance or post-disaster data collection, promote use of consistent measures, and build scientific knowledge regarding disaster effects. |
| Additional Considerations for Title V (“How can we create meaningful efficiencies…?”) | AMCHP | One-page .pdf document (link). | Guidance to ensure that jurisdictional Title V staff build EPR capacity in ways that can address federal reporting requirements. |
Learning Check: Module 3
Module 4: Establish/Promote EPR Communication about Target Populations with Clinical Partners, Public Health and Governmental Partners, and the General Public (Checklist Strategy #3)
Before starting this module, make sure you’ve downloaded and/or printed both the Checklist and Action Implementation Card for easy reference.
Overview
This video clip (1:36) introduces the presenters of subsequent related content and offers a “big picture” perspective on the significance of this strategy in building overall preparedness and response capacity. Presenter: Mikayla Frye, Program Manager for Workforce Development and Capacity Building, AMCHP.
Activities within Strategy #3 support one (2) PHEP capability:
- Information Sharing
- Community Preparedness
Didactic Breakdown of Select Activities
Watch the following video clips to learn about a few activities included in the checklist for Strategy #3. You can find the complete list of Checklist activities that support Strategy #3 in the Checklist document offered for download at the start of this course.
Centering Equity in Practice
Addressing maternal and infant health needs in planning for and responding to emergencies cannot be disconnected from the broader pursuit of equitable outcomes for all. This video clip (2:25) demonstrates how to apply an equity lens in implementing a specific capacity building activity (S3-A3). A primary takeaway is to continuously assess how women from racial, ethnic, and other identity-based groups that have been marginalized are being prioritized (or not) in processes, including the degree to which communication strategies meaningfully engage and focus on those communities most likely to be disproportionately impacted by emergencies. Presenter: Mikayla Frye, Program Manager for Workforce Development and Capacity Building, AMCHP.
Implementation Support Spotlight: Crisis and Emergency Risk Communication Framework
The following video clips (6:05 of total content) are excerpted from a presentation by Maria Rivera, MPH, CDC Health Communications Specialist. She focuses on the Crisis and Emergency Risk Communication (CERC) framework, which you can explore in more depth on this page of the CDC website. It provides access to a manual, training webinars, and related resources.
Supplemental Resources
| Title | Author(s) | Format | Purpose |
| CERC Templates and Tools | CDC | Interactive page (link) on a federal website. | Customizable documents to support health officials with communication throughout all phases of emergency management. |
| Communications section of Increasing Access to Contraception: A Toolkit for Program Development, Implementation, and Evaluation | CDC Foundation | Interactive page (link) on a nonprofit organization website. | Process guidance for developing and rolling out communications campaigns, leveraging examples from the Zika outbreak response. |
| Counseling Families on Disaster Preparedness and Infant Safe Sleep | CDC | One-page .pdf document (link). | Example of how public health communications can support clinical professionals and others poised to provide direct emergency response. |
| Natural Disaster Safety for Expecting and New Parents | CDC | Interactive page (link) on a federal website. | Example of targeted emergency messaging (across phases) for pregnant and postpartum people. |
Learning Check: Module 4
Module 5: Identify Public Health Programs, Interventions, and Policies to Protect/Promote Health and Prevent Disease and Injury in Emergencies among Maternal and Infant Populations (Checklist Strategy #4)
Before starting this module, make sure you’ve downloaded and/or printed both the Checklist and Action Implementation Card for easy reference.
Overview
This video clip (1:51) introduces the presenters of subsequent related content and offers a “big picture” perspective on the significance of this strategy in building overall preparedness and response capacity. Presenter: Mikayla Frye, Program Manager for Workforce Development and Capacity Building, AMCHP.
Activities within Strategy #4 support three (3) PHEP capabilities:
- Community Preparedness
- Public Health Laboratory Testing
- Public Health Surveillance and Epidemiological Investigation
Didactic Breakdown of Select Activities
Watch the following video clips to learn about a few activities included in the checklist for Strategy #4. You can find the complete list of Checklist activities that support Strategy #4 in the Checklist document offered for download at the start of this course.
Centering Equity in Practice
Addressing maternal and infant health needs in planning for and responding to emergencies cannot be disconnected from the broader pursuit of equitable outcomes for all. This video clip (2:28) demonstrates how to apply an equity lens in implementing a specific capacity building activity (S4-A2). A primary takeaway is to be intentional about reaching out to hospitals serving communities that have been made more vulnerable (by structural racism, geographic isolation, etc.) to the impacts of public health emergencies; their experiences can inform discharge protocols that can ensure the safety of all people who are pregnant and postpartum and newborns. Presenter: Mikayla Frye, Program Manager for Workforce Development and Capacity Building, AMCHP.
Implementation Support Spotlight: Creating Protocols and Continuity Plans
Please select either (a) hospital protocols for discharging newborns and postpartum women or (b) contingency plans for newborn screening to explore in more detail or choose to explore both if you are interested and time permits.
Hospital protocols for discharging newborns and postpartum women
EXPLORE: On the Hospital Preparedness Program (HPP) page of the Administration for Strategic Preparedness and Response (ASPR) website, you can learn about how this program is rolled out across jurisdictions (scroll to “Core Member Spotlights”) and access related resources.
WATCH: This video clip (6:48) is excerpted from a presentation by Kay Daniels, MD, Clinical Professor of Obstetrics and Gynecology at Stanford University. She frames her interest and experience in hospital preparedness, discusses the multiple layers of acuity and needs among maternal and infant populations in hospitals, addresses challenges associated with emergency transfers, and uses a wildfire example to underscore the need for standard evacuation, transfer, and discharge protocols.
Contingency plans for newborn screening
EXPLORE: The CDC’s National Contingency Plan for Newborn Screening (CONPLAN) is a detailed document that captures the vast newborn screening network in eight key strategic objectives and identifies challenges that may disrupt time-sensitive processes during and in the aftermath of public health emergencies.
WATCH: This video clip (5:45) is excerpted from a presentation by Sabra Anckner, RN, MSN, Associate Director for Clinical and Community Collaboration, AMCHP. She frames her interest and experience in newborn blood spot screening, uses a hurricane example to describe the process and what is needed to ensure continuity of operations during a disaster, and shares critical considerations related to the transportation and delivery of samples, communications with hospitals, and follow up support for families of children with an identified special health care need.
Learning Check: Module 5
Based on what you’ve learned, answer the following multiple-choice questions. When you click “submit,” you will see which of your responses were correct. For those questions you answered incorrectly, the correct answer will also be visibly indicated. For all questions, a brief statement justifying the correct answer will be provided.
Thank you for completing this course! We hope the content met or exceeded your expectations for learning and that the interactive components will support your readiness to champion maternal and infant health needs in preparing for and responding to future emergencies.
To receive continuing education (CE) credit for this course, click the button below to be directed to the CDC TRAIN platform where you will complete a brief post-test (and create a free account if you have not already registered for one). You must score 80% to pass and will only be allowed one retake.
Please contact workforce@amchp.org with any questions about the course or feedback for the architects.
| Where should my organization/agency start? What’s my role? The Application Activity on pages 1-2 of the participant workbook (see beginning of this course to download the fillable .pdf document) prompts you to use an impact matrix tool to select a priority activity within Checklist Strategy #2, #3, or #4 and determine individual action steps. The red buttons at the top right of each page are links to documents that can support your decision making. |